Benign Prostatic Hyperplasia (BPH)
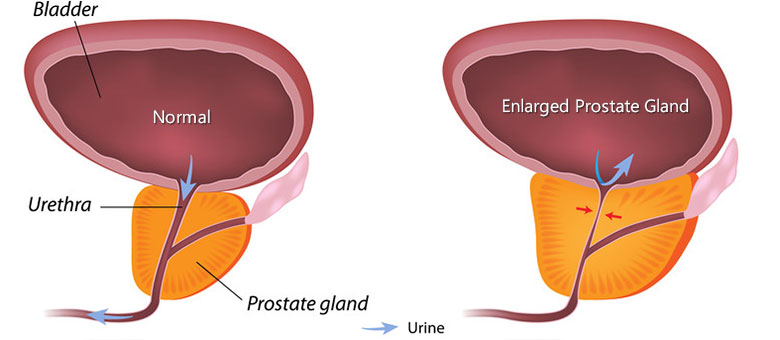
Benign Prostatic Hyperplasia (BPH) is a noncancerous enlargement of the prostate that may cause difficulty in urination. An enlarged prostate occurs commonly in men over the age of 60. Experts do not yet know what causes BPH, but the condition may be related to the hormone testosterone and its relationship to other hormones that changes during the aging process. The fact that the prostate begins to grow larger is not necessarily a problem. In fact, some men have extremely enlarged prostates but suffer no ill effects. On the other hand, some men have prostates that are only slightly enlarged and they suffer from bothersome urinary symptoms. These symptoms include difficulty urinating, the need to urinate quite frequently, or awaking during the night to urinate.
BPH treatment options
The enlargement of the prostate is known as benign prostatic hyperplasia (BPH) and may be due to hormone changes that men experience, although the exact cause is unknown. BPH is not cancer, and does not lead to cancer. Because BPH is rarely life threatening, treatment is usually required only if the symptoms are bothersome or if the urinary function is severely affected.
There are three major treatment options for BPH
- Medical therapy using prescription medications: Alpha-blockers and 5-reductase inhibitors are two common types of treatments used for benign prostatic hyperplasia (BPH). While they work differently on the prostate, both therapies work to relax the prostate to increase the flow of urine.
- Alpha-blockers work by relaxing the smooth muscle of the prostate and bladder neck to improve urine flow and reduce bladder outlet obstruction. Although alpha-blockers may relieve the symptoms of BPH to varying degrees, they usually do not reduce the size of the prostate. Alpha-blockers used to treat BPH include Hytrin® (terazosin hydrochloride, Abbott Laboratories), Cardura® (doxazosin mesylate, Pfizer Inc.), and Flomax® (tamsulosin HCl, Boehringer Ingelheim).
- Finasteride, a 5-reductase inhibitor, marketed under the name Proscar® by Merck & Co. Inc., works by actually shrinking the size of enlarged prostates. Proscar lowers the amount of the hormone dihydrotestosterone, which is a major cause of prostate growth. By shrinking the prostate, Proscar may gradually improve urine flow rate and decrease the symptoms of BPH.
For further information, including adverse events, please consult the appropriate prescribing information and your physician.
Alternative Therapy
A new trend is emerging in which patients are turning to vitamins, herbs, and natural remedies for BPH and other medical conditions. One such herb is saw palmetto, an extract that comes from the dried ripe fruit of the saw palmetto plant, Serenoa repens.
Beyond Medical Treatment
Some men may have enlarged prostates without any urinary symptoms. Physicians frequently choose watchful waiting as the best plan of action. For some patients, symptoms progress to a point where medical therapy is no longer effective. In those cases, patients may elect to have surgery.
Surgical Treatment
In spite of medical therapy, for some men the symptoms of BPH progress to the point where surgery may be necessary. For these men, there are a number of options to help relieve the pressure the prostate puts on the urethra.
TURP
A transurethral resection of the prostate (TURP) involves removing a portion of the obstructive prostate tissue by inserting an instrument called a resectoscope into the penis through the urethra. This procedure is usually done to relieve the symptoms of BPH and make urinating easier. It is performed to reduce the pressure on the urethra, which is being pinched by the enlargement of the surrounding prostate. This type of surgery has several advantages. Because no surgical incision is required, hospital stays are brief and recovery is usually uneventful. In a vast majority of cases, urinary function returns to normal after a TURP. In most cases, the ability to have sexual relations is also not affected by the procedure.
TUIP
A more limited surgical procedure -- transurethral incision of the prostate (TUIP) -- may be an option in some cases. TUIP, which is similar to TURP, is usually performed in men who have a relatively small prostate. In this procedure, an instrument is passed through the urethra to make a small incision in the prostate tissue to enlarge the opening of the urethra and bladder outlet, thus improving the urine flow rate and reducing the symptoms of BPH. TUIP is performed on an outpatient basis and usually does not require a hospital stay. Possible complications may include bleeding, infection, urethra stricture, and impotence.
Prostatectomy
Particularly if the prostate is very large, an open prostatectomy may be necessary. In this procedure, an incision is made in the skin of the lower abdomen so that the physician can remove the inner core of the prostate. Patients who undergo prostatectomy should expect at least a 2- to 3-day stay in the hospital, while full recovery can sometimes take up to 8 weeks. As with all major surgeries, prostatectomy patients may require a blood transfusion. Prostatectomy has become safer and less likely to leave men impotent or incontinent, although results vary from surgeon to surgeon. The risk of impotence, which is the inability to achieve or maintain an erect penis, often depends on a patient’s age and health. Incontinence, which is involuntary urination, appears to occur much less often than impotence in patients after radical prostatectomy.
Beyond Surgical Treatment
Some men may have enlarged prostates without any urinary symptoms. Physicians frequently choose watchful waiting as the best plan of action. For some patients, symptoms can be effectively controlled through the use of medical therapy.
Active Surveillance
Watchful waiting, an option in which a physician monitors the symptoms of BPH but chooses not to treat immediately. Clinical studies have shown that the symptoms of BPH can sometimes wax and wane and even improve on their own. For that reason, if a man’s BPH symptoms are not severe enough to be bothersome, he and his physician may choose a program of watchful waiting. It involves a yearly or twice-a-year exam by a physician to carefully monitor the progression of symptoms and possible complications. These complications may include urinary retention, infection, blood in the urine, or damaging backup of urine into the kidney.
